Celiac & Gluten Related Disorders
Celiac disease is an autoimmune disorder that often runs in families. When someone with celiac disease eats gluten, the body causes an immune attack on the intestinal lining. Gluten is a protein found in wheat, barley and rye. Some breakthrough findings were made in 2011. Research found that celiac disease is just one piece in a spectrum of gluten-related disorders. The spectrum also includes non-celiac gluten sensitivity, which has many of the same symptoms as celiac disease, and wheat allergy. In this article, you will find basic information on three gluten-related disorders: celiac disease, non-celiac gluten sensitivity and wheat allergy.
What are gluten-related disorders?
The spectrum of gluten-related disorders refers to all conditions related to gluten, the protein found in all forms of wheat, rye and barley. They include celiac disease, wheat allergy, and non-celiac gluten sensitivity.
What is celiac disease?
Celiac disease is an autoimmune disorder that often runs in families. It affects nearly 1% of the population or about three million Americans. Since 1950 celiac disease has increased four-fold. When someone with celiac disease eats gluten, the body causes an immune attack on the intestinal lining. This harms the lining and prevents nutrients from being absorbed into the body. This leads to nutritional deficiencies and related health problems and symptoms.
Doctors and scientists are currently conducting research and exploring several different theories as to what causes celiac disease. At this time, we know that in people who have the genes needed to develop celiac disease and who are eating gluten, a particular event can activate, or "turn on," this autoimmune disease. In some cases, stressful events like pregnancy, surgery, infection or severe emotional distress can trigger the onset of celiac disease.
The only treatment for celiac disease is a strict lifelong gluten-free diet. Although it can be challenging at first, individuals can learn to love the gluten-free diet. In fact, the gluten-free diet becomes a routine, a part of life.
Because celiac disease can mimic other diseases, such as irritable bowel syndrome, it can be difficult to receive a prompt and accurate diagnosis. Unfortunately, 95% of people with celiac disease may currently be undiagnosed or misdiagnosed with another condition. Those without a diagnosis are more likely to have bone disease such as osteoporosis, reproductive health problems like infertility, some cancers and an overall increased risk of early death.
What is wheat allergy?
Wheat allergy includes a spectrum of immune responses involving histamine that occurs within minutes to hours after wheat exposure. Typically, any one or a combination of skin, gastrointestinal, and respiratory systems undergoes the effects of food allergy. Along the spectrum, classic food allergy, wheat-dependent exercise-induced anaphylaxis (WDEIA) and wheat dependent aspirin-induced anaphylaxis (WDAIA) are included. We know that in some individuals, particularly with WDEIA, protein components in rye and barley can cross-react with gluten, thereby indicating the need to avoid gluten and not just wheat. Therefore, some individuals with a wheat allergy may need to follow a gluten-free diet too.
Allergic sensitivities, including those to wheat, can be diagnosed by skin prick testing or blood tests such as Wheat IgE. Both IgE and skin prick tests will indicate a sensitivity to wheat or other foods. However only a food challenge will confirm your body's response. A food challenge should only be performed by a trained medical professional in the right setting. Individuals who have gluten-related symptoms but test negative for a wheat allergy may have non-celiac gluten sensitivity.
What is non-celiac gluten sensitivity?
The research on non-celiac gluten sensitivity is only just beginning. Doctors estimate that up to 6% of the population is affected. Non-celiac gluten sensitivity is thought to mostly affect adults.
Non-celiac gluten sensitivity can be used to describe persons who experience symptoms similar to celiac disease because they, too, cannot tolerate gluten. However, non-celiac gluten sensitivity does not cause the same type of bodily response as celiac disease. Early research suggests that the body of a person with non-celiac gluten sensitivity acts to fend off an attacking substance but does not result in intestinal damage. Because of their shared symptoms, it's important that your doctor test for celiac disease and rule it out before considering non-celiac gluten sensitivity.
Unlike celiac disease, non-celiac gluten sensitivity does not appear to be genetic and it is not thought to cause long- term health complications.
At times you may have heard "gluten sensitivity" or "gluten intolerance" to describe what has recently been established as non-celiac gluten sensitivity. These terms are now discouraged. It is important to keep this in mind as you read health information presented online and in the media.
How are gluten-related disorders diagnosed?
The diagnoses of celiac disease, non-celiac gluten sensitivity and even wheat allergy all start with the simple collection of a blood test.
Your doctor may order blood tests to help see if you have a gluten-related disorder. These conditions include celiac disease, wheat allergy and non-celiac gluten sensitivity. Let's visit each condition separately so that you can learn what to expect if your physician starts this process.
Celiac Disease Diagnosis
Celiac disease is an autoimmune disorder that often runs in families. When someone with celiac disease eats gluten, the body causes an immune attack on the intestinal lining. Gluten is a protein found in wheat, barley, and rye, and their by-products. Blood tests and a medical history taken by a medical professional are the first steps in a diagnosis of celiac disease. A blood test will measure your body's response to gluten. Please note that in order for the blood tests to be helpful to your doctor, you must be eating a normal, gluten-containing diet.
- Total immunoglobulin A (Total IgA)
- Immunoglobulin A – Tissue Transglutaminase (IgA-tTG)
- Immunoglobulin A – Endomysial Antibody (IgA-EMA)
- If the individual is deficient in IgA, it is recommended that Immunoglobulin A / Immunoglobulin G-
- Deamidated Gliadin Peptide (IgA/IgG-DGP) also be ordered.
Your doctor may order one or more of the following laboratory tests to begin the diagnosis of celiac disease:
The IgA-tTG test can identify many adults and children who have celiac disease. The test is widely available and cost effective, too. If your blood test is positive, your physician may refer you to a gastroenterologist. This doctor may perform an upper gastrointestinal endoscopy. This medical procedure will allow your doctor to take a sample of your small intestine to see if you have celiac disease. You must also be on a normal, gluten-containing diet before this procedure in order for your doctor to tell if you have celiac disease. (So if you learn that you have a positive celiac disease blood test and are tempted to go on a gluten-free diet, think again.)
Special note:
Although the IgA-tTG test is very helpful in identifying many individuals who have celiac disease, this blood test is not perfect. If your blood test is negative and your doctor remains suspicious that you have celiac disease, your doctor may consider using another blood test to determine if you do have this condition. For example, if an individual has a moderate to high risk of celiac disease but a normal IgA-tTG, a doctor may use the IgA-DGP blood test to guide a decision regarding the need for an endoscopy. This is because some research shows that individuals with a normal IgA-tTG but who test positive for IgA-DGP do in fact have the intestinal damage typical of celiac disease.
What should I expect during an endoscopy?
An upper gastrointestinal endoscopy is a very safe and routine procedure. There are some things you will need to do to prepare for the procedure. Your doctor will talk about these important details with you. You may be lightly sedated during the procedure. The actual endoscopy only takes about 15 minutes. During the endoscopy, your doctor will use a small camera to look at your intestinal wall. Your doctor will be looking for damage or flattening of the villi (small fingerlike projections that help to absorb nutrients from food). A few small samples will be taken to review under a microscope to confirm a diagnosis of celiac disease.
What should I do if I'm already eating gluten-free?
If your doctor suspects that you have celiac disease, and you are already on a gluten-free diet, he or she may suggest a gluten challenge. This will help your doctor give you a more definitive answer and also confirm whether the gluten-free diet is helping you.
How is genetic testing helpful in the diagnosis of celiac disease?
Celiac disease is a genetic condition, which means that it often runs in families. Genetic testing can be useful in certain situations when it comes to the process of diagnosing celiac disease. Genetic testing cannot diagnose celiac disease, but is a tool that can rule it out.
Genetic testing is useful for individuals who are already on a gluten-free diet if their doctor thinks they may have celiac disease. It is also useful to test family members of persons with celiac disease. Because celiac disease runs in families, first and second-degree relatives are at an increased risk for the disease.
The test will identify whether the individual has the genes associated with celiac: HLA-DQ2 and HLA-DQ8. If a person doesn't have either of these genes, the likelihood of celiac disease is very low.
If you test positive for the HLA-DQ2 or DQ8:
This would indicate that you have a risk for developing the condition. However, it is important to know that many healthy people without celiac disease also have one or both of these genes. (Up to 40% of the population has these genes). You should discuss the next steps with your doctor.
If you test negative for the HLA-DQ2 AND DQ8:
This would indicate that you are very unlikely to develop celiac disease.
Non-Celiac Gluten Sensitivity Diagnosis
Non-celiac gluten sensitivity has many symptoms that overlap with celiac disease. So, it is impossible for doctors to decide if you have this disease based only on symptoms. At the current time, there are no laboratory tests to see if you have this disease. This is important to remember since some laboratories claim to diagnose non-celiac gluten sensitivity.
In order to diagnose non-celiac gluten sensitivity doctors may first rule out celiac disease and wheat allergy. Then, doctors may put the individual on a gluten-free diet to see if symptoms go away. If symptoms go away, they may then have the individual undergo a gluten-challenge. A doctor will decide you have non-celiac gluten sensitivity if the gluten challenge shows that a gluten-free diet makes you better.
Wheat Allergy
A doctor can decide whether you have a wheat allergy based on one of two ways: a skin prick test or a blood test, such as Wheat IgE. Both tests are very accurate.
During a skin prick test, a drop of the allergen is placed on your forearm or back, and your skin is pricked so the allergen can enter your skin. This is done for each of your suspected allergens. If you are allergic to any of the substances, you'll have a reaction such as itchy, red bumps. During the Wheat IgE test, a single sample of your blood is drawn from your arm. Using this sample, the laboratory can test your body's reaction to hundreds of different allergens. Your doctor will decide which allergens to test. In this case, your doctor can test for wheat.
If you have symptoms of a gluten-related disorder, don’t head for the grocery store to start a gluten-free diet. First, go see your doctor.
Gluten-related disorders such as celiac disease and non-celiac gluten sensitivity are treated with the gluten-free diet. “Gluten-free” has become a staple in the headlines for news segments, magazines and newspapers in recent years. Celebrity attention has made gluten-free the newest diet craze. Other articles talk about how a gluten-free diet helped reduce symptoms the author had been experiencing for months or even years. So, it can be tempting to take treatment into your own hands. But instead, first get the proper education and counselling from your doctor or other trained healthcare professional.
Here are some reasons to see your doctor before going gluten-free:
Your Test Results Won’t Be Helpful
One important reason to see your doctor before starting a gluten-free diet is that lab test results ordered by your doctor may not reflect your condition. Why? Because the blood tests for celiac disease can only pick up the disease when the trigger – gluten – is in your blood. And the only way it can be in your blood is if you eat it. If you start a gluten-free diet before you see your doctor, you may have to go back to a normal, gluten-containing diet in order to receive an accurate diagnosis.
You May Miss The Real Diagnosis
It is important to get an accurate diagnosis from your doctor. If you don’t, you run the risk of treating a disease you don’t have, or worse, missing a more serious condition. Other conditions that have similar symptoms include Crohn’s disease, bacterial overgrowth, intestinal lymphoma and lactose intolerance. Also, the gluten-free diet is not only hard to navigate, but it’s two to three times more expensive than a regular diet. It can also greatly impact a person’s quality of life, including their social and professional lives and psychological well-being. Gluten-free isn’t for everyone.
Important Dietary Concerns
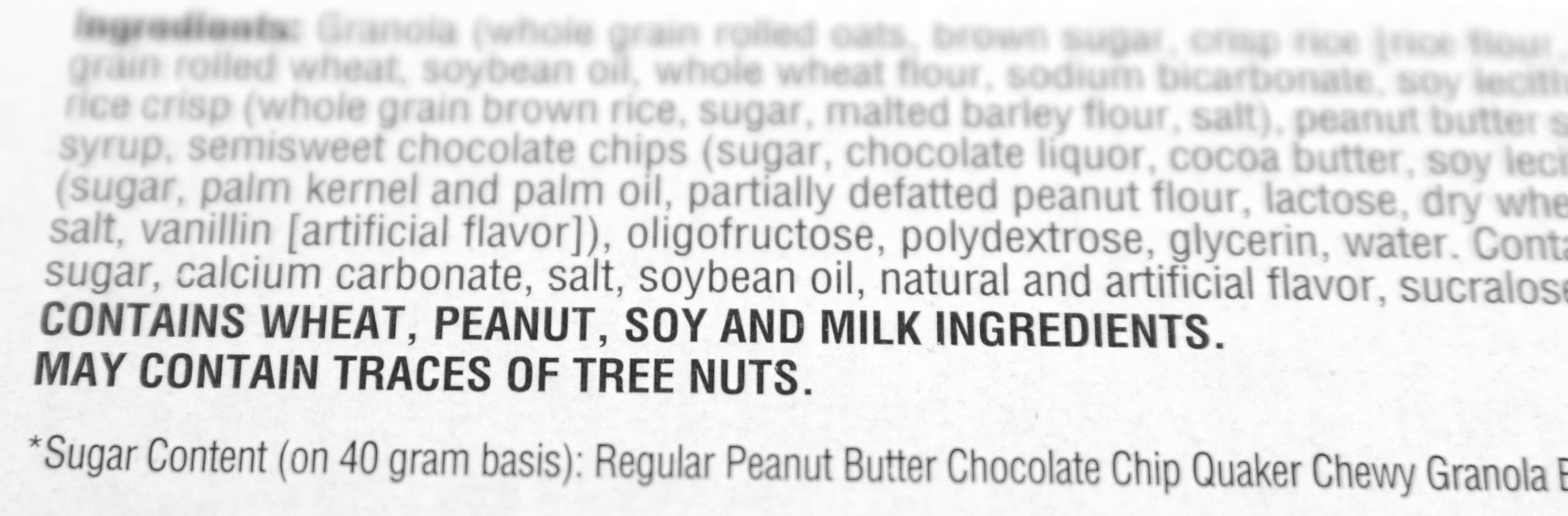
Once you are diagnosed with celiac disease, you should talk with a dietitian or a nutritionist who knows about the gluten-free diet. This is one of the five key elements in the National Institutes of Health’s (NIH) recommendations for the management of celiac disease. Starting the gluten-free diet can be challenging. People with celiac disease must strictly follow the gluten-free diet for life. It means eliminating all forms of wheat, barley and rye, ingredients found in many common foods such as bread and pasta. Gluten can hide in other foods too, such as soy sauce and liquorice. A knowledgeable dietitian or nutritionist can help you learn to read labels and inquire about ingredients so that you don’t miss something and accidentally eat gluten. Because even a small amount of gluten can cause intestinal damage in a person with celiac disease, it is critical that you strictly follow the diet.
Additionally, a dietitian or nutritionist can help you and your family to create a healthy gluten-free diet This is particularly important because many gluten-free products are not fortified with important nutrients such as B vitamins, calcium, vitamin D and zinc. In fact, many packaged gluten-free products are high in fat, calories and sugar! As a result, those eating gluten-free may suffer from nutrition deficiencies, which may create health problems in the future.
Finally, a dietitian or nutritionist can also share tips on how you and your family can make your kitchen gluten-free friendly. It is important that you and your family know that shared food products and kitchen appliances and utensils can make you sick if cross-contamination occurs. A dietitian or nutritionist can help you to learn the “in’s and out’s” of eating gluten-free safely within your own home.
Celiac Disease Requires Proper Follow-Up
Celiac disease has increased fourfold since 1950. Doctor’s don’t know why the disease is on the rise. If left untreated, people with celiac disease are at risk for developing complications such as bone disease, reproductive health problems, and premature death. Therefore, it is important for individuals and physicians to work together to diagnose and manage this condition. Only about 5% of the people with celiac disease have a formal diagnosis. The gluten-free diet is by no means a cure all. Individuals who truly have celiac disease but are not diagnosed by a doctor may not receive the proper follow-up with a medical professional. This may put them at risk for accidental gluten exposure, low levels of vitamins and minerals and other future health complications. The bottom line is this: if you think you have celiac disease it’s best to go see your doctor and get tested. Today’s blood tests are widely available, cost effective and accurate.


